March 18, 2021
How often do you think about your breathing? Well, you’re probably thinking about it now that it’s been mentioned, but normally your lung function is completely involuntary. You go through your daily activities without having to think about conscious respiratory function or breathing habits. The respiratory system of healthy individuals is truly incredible, as it monitors oxygen levels in all different parts of the body. However, there are cases where this cognition can be disrupted, and you can experience shortness of breath, inflammation, or airflow obstruction that can disturb your quality of life. One of these cases is known as chronic obstructive pulmonary disease.
Chronic obstructive pulmonary disease is more commonly referred to as COPD and is defined as an inflammatory lung disease that slowly progresses and blocks airflow to the lungs. A COPD patient doesn’t have normal lung function and will experience difficulty breathing or more severe symptoms. Depending on the severity of your diagnosis of COPD, you may need different treatments to reduce risk factors for other disorders, deficiency, and illnesses. While the symptoms of COPD can affect your life, there are treatment options to help improve your quality of life and reverse the progress of the disease.
As with any serious health condition or burden of disease, a better understanding of your diagnosis is half the battle. So if you’ve been experiencing fatigue, shortness of breath, chronic cough, or trouble with lung function, you may need to learn more about what chronic obstructive pulmonary disease is all about.
What is COPD?
At its core, COPD is a cluster of diseases that all affect the lungs, your ability to breathe, and your overall health status. A primary cause of COPD is either emphysema or chronic bronchitis, which we’ll talk about a bit more later. Millions of Americans suffer from COPD exacerbation while many may not even realize that they have COPD. While it is serious for your health status, there are ways to treat COPD, so that you still have maximum functional capacity. Stable COPD means that you can continue living your routine activities without breathlessness. This will also reduce the likelihood of an exacerbation.
Effect on the Lungs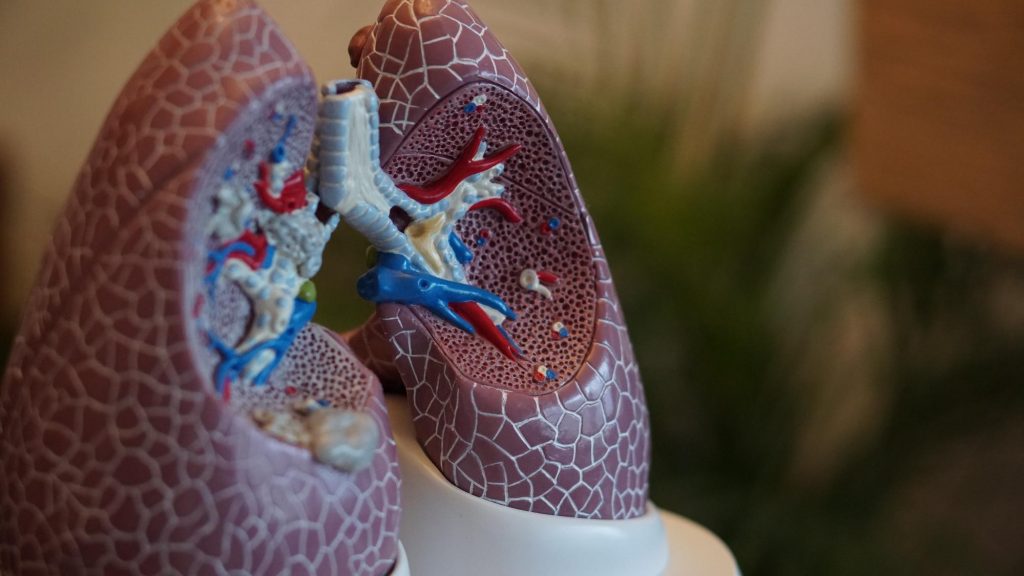
You probably learned about the function of your lungs and lung function change in elementary school health class, but a refresher never hurts. When you take a breath, functional capacity air travels down your trachea, which splits into the two bronchi which separate into many different little tubes called bronchioles. From there, the air sacs called alveoli fill with oxygen and pass that oxygen into the bloodstream through tiny blood vessels. This gas exchange allows oxygen in and lets carbon dioxide out. These air sacs and bronchial tubes need to be flexible and have elasticity. For a patient who suffers from COPD, these air sacs tend to over-expand from hyperinflation and trap air inside your lungs. This can cause chest tightness, severe cough, or other respiratory symptoms.
What contributes to COPD?
If COPD is a collection of different kinds of lung disease, it helps to know exactly what those airflow obstructions or issues are. Most prevalent COPD disease progression is a result of emphysema or chronic bronchitis.
Emphysema
Remember those air sacs we were talking about earlier? These are known as alveoli. Emphysema harms alveoli and leaves them weak, damaged, or broken. This means oxygen has much more trouble getting from the lungs to the bloodstream. The variables of this condition can cause airflow limitation, especially during physical activity, and it can lower your exercise capacity. Risk of exacerbation may mean low blood oxygen levels. Collapsed air sacs will also mean you’ll experience breathlessness because you can’t get irritants and carbon dioxide out of your lungs.
Chronic Bronchitis
While emphysema deals with alveoli, your bloodstream, and blood vessels within the lungs, chronic bronchitis is more about the bronchi themselves. This lung infection is a result of inflammation within the bronchial tubes. This, combined with added mucus or phlegm production, has a significant relationship to breathing problems and blockage of airways. These narrow tubes will lead to a chronic cough that remains prevalent no matter how many times you clear your throat during the daytime.
Causes of COPD
COPD is typically a disorder that affects a majority of individuals of older years of age. Lung damage can be a result of a few different factors and exacerbation rates, the most common of which is smoking. Inhaling any dangerous fumes, pollution, and even some pollens can also cause COPD exacerbation, as can an acute illness such as a cold or flu which temporarily inflames the lungs.
Smoking
Tobacco smoke affects your lungs and respiratory health. Cigar or cigarette smoke, pipes, e-cigarretes, vapes, or being exposed to secondhand smoke increases susceptibility that those toxic elements are getting trapped in your lungs and affecting your airways. If you’re a long-time smoker, you’re at higher risk of developing COPD than nonsmokers, and the disease progression will only get worse until you are at risk of death. It may be time for an intervention to quit smoking and give your lungs a break from the exacerbation of COPD.
Inhaling Dangerous Fumes
Unfortunately, not everyone gets to avoid dangerous fumes or dust particles. In homes with poor ventilation or air pollution, people may inhale toxic chemical fumes while cleaning or cooking. You may also have a job where you are at a higher risk of inhaling these toxins because of failures in mechanical ventilation. Long-term exposure to gases and chemical fumes in the workplace can cause mild COPD, an early onset of symptoms, or exacerbation of the problem. If you are able, look for a job with an endorsement from a healthcare provider that the worker’s conditions won’t have a negative impact on your health.
Genetics
Your genetics can also place you at higher risk of developing COPD. Some individuals have a genetic condition where they have low levels of the alpha-1-antitrypsin protein which helps protect the lungs. Due to this alpha-1 antitrypsin deficiency, studies show that these patients may develop emphysema or liver diseases. Check with your family members and provider to see if your stage of the disease could be a result of this.
Asthma
While asthma is not necessarily a cause of COPD, it is a risk factor to be aware of. Individuals who already have trouble with breathlessness, wheezing, or breathing problems should be especially aware of the impact of COPD symptoms. Avoid smoking and work with your medical provider to keep you asthma under control to avoid severe exacerbation of your lung problems.
Symptoms
Depending on the exacerbation of COPD, you will experience different symptoms. During the early stage of mild exacerbation, you may not even realize you have the disorder. It may just feel like you have a cold, influenza, or bronchitis. A healthcare provider can help you decide if your symptoms are severe enough to be a sign of COPD through observational study and other tests. Early intervention is the only way to slow your COPD symptoms before they get worse.
Once you do start experiencing an impact of COPD symptoms, they can be quite varied. From early symptoms to more advanced issues, stay on top of your personal experiences and side effects. The most common symptoms include:
- Shortness of breath
- Breathlessness during physical activity
- Lower exercise tolerance
- Wheezing
- Chest tightness or chest pain
- Chronic cough
- Constantly coughing up mucus or phlegm
- Respiratory infections or sore throat
- Viral infections or bacterial infections
- Fatigue
- Lack of energy
- Unexpected and unexplained weight loss (during later stages)
- Swelling in your lower limbs (during later stages)
You may experience these symptoms regularly, or you may have severe episodes where you need to visit a clinical practice or even resort to hospital admission. If you find your symptoms of COPD are not improving with treatment, you‘re experiencing an infection or change in your sputum, or you are constantly in a daze, it is time to call your clinician or caregiver for an official prognosis.
Further Complications of Severe COPD
While COPD itself can be managed relatively easily, it can also lead to more serious side effects or complications that will affect your health-related quality of life. COPD puts you at higher risk for opportunistic infections like pneumonia, which can cause further damage to your already unstable lungs. Because your lungs and your heart are so closely connected, observational studies have shown that a history of COPD can lead to heart disease, heart failure, or high blood pressure. Without regular treatment, a number of studies say you may also find yourself feeling depressed as a symptom burden of not being able to breathe. Even if you have mild COPD, it can lead to a more severe disease that could end up having negative effects on your lifespan or mortality rate. COPD can even be a common cause of death.
Getting a Diagnosis
If you decide to make an appointment with a clinician, pulmonologist, or healthcare professional about your symptoms, there are a few different prospective studies they will to do diagnose you with COPD. Because COPD symptoms often appear as mild respiratory symptoms, you may not get a full diagnosis until the disease is a severe exacerbation of COPD. There are a few different ways a healthcare provider will diagnose you with COPD.
Spirometry Testing
The gold standard test of pulmonary function is called spirometry. This simply involves taking deep breaths into a tube to measure the baseline of your lung capacity and seeing the respondent variables.
Image Testing
The next step may also involve a chest X-ray or CT scan. This will give you a more systematic review of your lungs, blood vessels, and heart. Test results can also help detect lung cancer or other serious lung problems.
Stages of COPD
Just like any disorder, there are stages of COPD. In the early stage, you should be able to live a healthy lifestyle with few breathing issues. There are four official stages: mild, moderate, severe, very severe. The disease process or unreported exacerbation could end in much more serious complications like heart disease, lung cancer, or depression and anxiety.
Treatment Options
Once you have an official COPD diagnosis, it’s time to get to work on recovery and treating your individual symptoms. You can take a few different pathways or lifestyle changes depending on the progressive disease and your treatment goals.
Medication
There are medications and steroids that can help you deal with your group of symptoms. Bronchodilators come as inhalers and can help relax the muscles around your airways. This dose inhaler can be taken when you experience a flare-up of COPD symptoms. You can also inhale oral corticosteroids for longer-lasting relief. Aside from just inhalers or bronchodilators, you can also benefit from antibiotics and oral steroids during flare-ups.
Oxygen Therapy
For more severe COPD cases where you have gone through hospitalization, you may need oxygen therapy vs. antibiotic therapy moving forward. This involves carrying a lightweight oxygen assistance device that helps increase your blood oxygen levels. Depending on your disease prognosis, you may only need this at night time or during the worst parts of the day. This is one of the proven therapies to help lengthen your life if you have a COPD diagnosis.
Reducing Your Risks
Living with COPD can change your quality of life. Before you get to that course of the disease, it can help to reduce your risks altogether using a few different methods.
Quit smoking.
First and foremost, chronic smokers should take steps to quit. Constantly inhaling toxins in high doses can be detrimental to the health of your lungs and pulmonary function. The best thing you can do is give up smoking for good.
Maintain your overall health.
Your body is incredibly interconnected. A healthcare provider will tell you that taking care of your health overall will help your lungs. This means they don’t have to work as hard to get oxygen to the rest of the body.
Get flu shots.
COPD can be aggravated by other serious colds, the flu, or pneumonia. Prevent these risks by always getting your influenza vaccine and lowering other risk factors.
Exercise regularly.
Your lungs function just like a muscle. If you aren’t working it out, it may start to weaken. Regular exercise can help improve the strength of your lungs and stop deterioration.
Consult your doctor.
Of course, if you’re worried about your risk of COPD, it is always a good idea to talk with your doctor about ways you can reduce your risk factors.
DISCLAIMER
The information featured in this site is general in nature. The site provides health information designed to complement your personal health management. It does not provide medical advice or health services and is not meant to replace professional advice or imply coverage of specific clinical services or products. The inclusion of links to other web sites does not imply any endorsement of the material on such websites.
